Case studies - Lavori scientifici
Specific use of the implant stability quotient as a guide to improve healing for patients who had undergone rehabilitation with fixed implant-supported dental prostheses
Case studies - Lavori scientifici
The Management of Advanced Lateral Bone Defects with the Splitted Bone Block Technique in the Maxillary and in the Mandible. A Follow-up until 8 Years
Trasarti Stefano and Marroni Daniela
Abstract
In the last years, the fixed restoration with dental implants has become increasingly widespread, due to the predictability and the development of implant therapy. This has generated in the patient an increase of expectations as for the aesthetic and function. Often the surgeon has to treat situations that requires an increase of the bone in order to place the implants in a correct prosthetic position. This study evaluated the treatment of the advanced lateral bone defects using only autogenous bone and the following period up to eight years.
Introduction
Following tooth loss, deficiencies in alveolar ridge bone height and width may limit the use of dental implants. To ensure an aesthetic and functional rehabilitation in the long term, the reconstruction of the bone loss represents a big challenge, particularly in the case of advanced bone lost. Clinically, the greatest loss of alveolar ridge is usually in the horizontal dimension. Ridge augmentation has been adopted for functional and aesthetic implant-supported restoration of a atrophic, narrow alveolar process. Bone grafting with autogenous bone in block, guided bone regeneration(GBR) and ridge expansion techniques have been used for this purpose. GBR is a predictable surgical procedure for lateral ridge bone augmentation that results in enlargement of the alveolar crest in partially edentulous patient. However these procedures have disadvantages such as unpredictable bone resorption and the difficulty with soft tissue closure resulting in a risk of wound dehiscence [1, 18]. An alternative method for lateral bone augmentation is the split crest where the crestal bone is split to obtain a width sufficient for implantation [1, 19]. This method can be used to correct horizontal defects in the crestal region; fixation of the split bone is usually not necessary. This technique can be performed when we have a thickness in the rest of bone in the presence of spongiosa. The present article describes a procedure named “splitted bone block technique” according to Khoury’s concept [9-10], that using only autogenous
bone can reconstruct the correct thickness of the bone, independent of the residual bone thickness, without using biomaterial or membrane [8, 9]. In this study we want to evaluate the predictability over the years of this technique, selecting only cases, where the residual bone was maximal 3mm in the thickness. The goal was to evaluate the quality and the resorption of the new bone in these extreme atrophied lateral bone.
Some of these defects were resulting after previous extracted infected teeth, periodontal disease or fracture of tooth after an accident. In six cases, the bone atrophy was the result of unsuccess with previous different techniques using biomaterials.
Materials and methods
We evaluated 22 consecutive patients with advanced lateral bone defects in the maxilla and in the mandible. The inclusion criteria were the residual bone thickness in single tooth area maximal until 3mm and we excluded defects where the residual bone thickness was more than 4 mm. In all the cases it was essential to proceed to bone augmentation before to insert implants, due to the advanced bone lost (average 2mm). All the patients had a high demand because they wanted to be rehabilitated as fast as possible with the guarantee of result over the time.
In the most of the cases we had to rebuild only one wall (palatinal/lingual or vestibular) and in six cases we had the lost of both walls. To all the patients it was illustrated and explained the necessity of the bone augmentation before the implant placement. Another inclusion criteria was to selected only cases where It was not possible to insert the implant at the same time of augmentation due to advanced bone lost. All the patients were operated under local anaesthesia.
We proceed with the analysis of the case with models, X-ray and clinical views (Figures from 1 to 6).

Figure 1: Preoperative frontal view

Figure 2: Preoperative frontal view with big lateral defect


Figure 3 and 4: plaster model occlusal and frontal view.


Figure 5 and 6: X-ray preoperative
Before to proceed to bone harvesting, it was required to all the patients an orthopantomogram and a CBCT to register anatomical landmarks and to estimate the bone atrophy.
All the augmentations were carried out according to Khoury's biological concept. The harvested bone block from the mandibular retromolar area was collected with the Microsaw (FRIOS DENTSPLYSIRONA), splitted in two thin blocks (Figures 7, 8 and 9) and at the end was screwed to reconstruct the bone wall (Figure 10). The space between the remaining bone and the new wall was filled with only particulate bone chips gained by scraping the blocks until a thickness of 1mm. The blocks were fixed with Microscrew (Stoma, Tuttlingen) on distance to the remaining alveolar bone to rebuild the correct thickness of the native bone (Figure 11). No membranes were used and we closed the wound after realising the periosteum to ensure a primary closure of the area.

Figure 7: lateral bone defect with only 1 mm thickness.

Figure 8: Harvesting bone block.
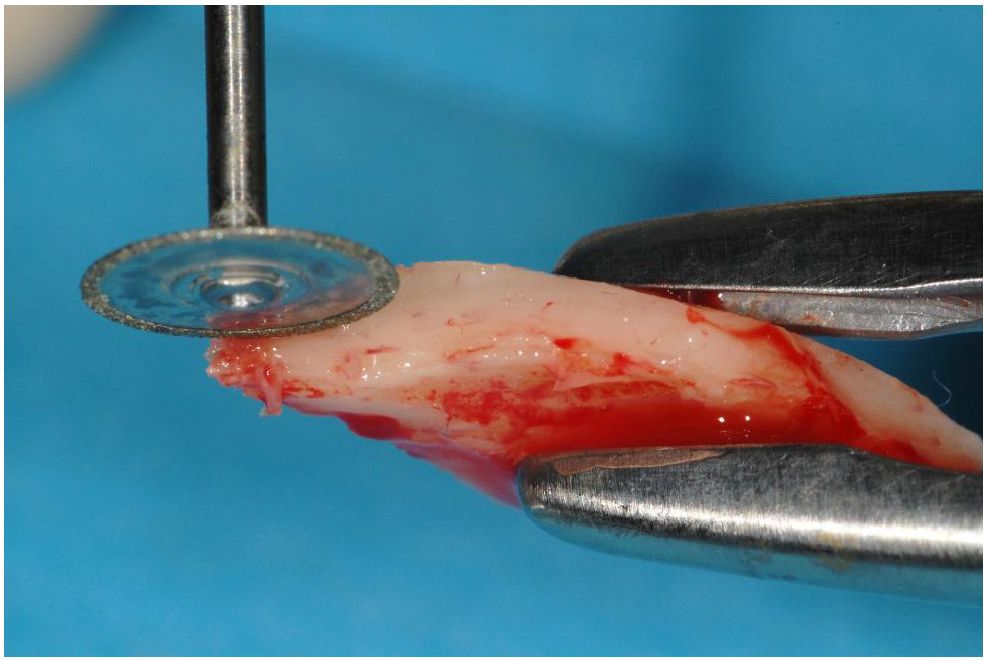
Figure 9: Cutting bone with the Microsaw.

Figure 10: Block screw on distance.

Figure 11: Bone reconstruction.
The patient was instructed to post operative treatment. They received for one week Antibiotic Amoxicillin 1g per os for one week, Ibuprofen 600mg for three days and Chlorexidine 0,2% for two weeks. In all the 22 patients the post operative wound healing was inconspicuous and painless, but with a 5 days lasting swelling.
Results
After only 3,5/4 months we proceed to implant insertion. The regenerated bone showed good volume and healthy soft tissue (Figure 12).

Figure 12: Clinical view after 3 months.
Under local anaesthesia we proceed to implantation. The grafted bone showed a good revascularization and a stable bone volume with the same consistence and bleeding of the native bone. Therefore, we proceeded to insert 22 implants with regular diameter (3,4 -3,8mm) XIVE Implants, (Dentsplysirona) and length (9,5- 11 mm) in the augmented area in the mandible and in the maxillary. 12 cases were performed in the maxilla and 10 in the mandible.
The primary bone width at the beginning was 1- 3mm in average and it was increased at the end of the
surgery until a thickness of 7,5mm in average. The thickness of the grafted crest 3 months postoperative demonstrated not resorption and stable bone, permitting to insert all the planned implants without further bone management. No healing problems like dehiscence or necrosis occurred.
After 3 months in 18 patients we proceed to second stage surgery with additionally a free connective tissue graft. We proceed with an apical position flap in conjunction with connective tissue graft. In this way we were able to increase the volume and the keratinized gingiva to improve both the aesthetics and the function. After one month (Figure 13) we proceed to the provisional rehabilitation with the prefabricate Tempbase caps for Xive implants. This Temp-base permit us to make with the caps a fast provisional crow to conditionate the gingiva.

Figure 13: Healing after the second stage surgery.
After 3 months, the definitive crowns was made (Figure 14)

Figure 14: Definitive crowns.
The patients were regularly controlled between 3 and 8 years. Each year it was registered the probing around the implant and regularly repeated a new X-ray. The follow-up after 8 years of loading showed the really good aesthetic and functional result with stable tissue (Figures from 15 to 18). All the patients presented a
satisfied functional and aesthetic result. The radiographic control documents the stability of the grafted and regenerated bone over the years (Figure 19).



Figure 15 to 17: Follow-up after 8 years


Figure: 18 and 19: Xray after 3 years and after 8 years.
Discussion
The implant rehabilitation in the patients with insufficient bone volume and quality represents a big challenge in the implantology. The reconstructions of the bone defects can be perform with different approaches as described in the literature [1, 3, 4, 13- 15]. Todays the autogenous bone is considered the gold standard particularly for the predictability of these reconstructions [9, 13, 16].
The correct position in 3D dimension of the implant requires a good bone dimension as in the width as in the height. The implant position in the not augmented bone always causes problems due to the position and not correct inclination of the implant resulting in an anaesthetic result and difficulties for the prosthetics rehabilitation, particularly in the aesthetic area [3, 5].
In the last years were described very well different techniques in the bone augmentation to the goal to rebuild the bone defect. To these methods belongs the use of biomaterials (alone or in combination with autogenous bone) or with the combination with resorbable or not resorbable membrane [1, 3, 13, 15].
Other techniques are the GBR (Guided Bone Regeneration) or the use or bone block [2, 7, 9, 16].
Very relevant is the use of the autogenous bone that we have to differentiate between the use as compact bone block or the shell technique [8, 9].
However, it has been widely demonstrated that autogenous bone grafting is the most predictable method for achieving optimal bone size and insertion site quality, especially for larger bone defects [4, 7, 16].
In all the 22 patients we reconstructed the bone defects following the Splitted-Bone -Block Technik as described by Prof Khoury [8-10]. In all the selected patient we collect autogenous bone from the retromolar area and we cut into two parts. Each part of the bone was reduced in very thin thickness with a Safecraper (META) to permit at the same time to collect particulate bone chips. One piece of the bone was screwed to the lateral part of the defect to repristinate the thickness of the bone and the space was filled with poor autogenous particulate bone. The separated and thin bone block functions like a biological membrane, while the particulate bone simulates the spongiosa area like we have in the nature. The big advantage of this method is the reduction of the rehabilitation time because after 3-4 months, we are able to put the implant finding really bone. The quality of this bone is really similar to the native bone. Another relevant aspect for the stability and the predictability is the quality of this regenerated bone around the coronal part of the implant where the most of loading comes [14].
This is value for the small defects like reported in this article but also in the big ones.
Another advantage with this technique is the vitality of the bone that is well demonstrated also with histomorometric exams [9]. All these patient have showed in the following-up period a stable result. The described method in the presented article shows the result and the predictability over the time in the presence of bone defects, which with another techniques not so easy to dominate is. In this way the clinicians can manage similar defects in small time and with good predicibility over the time.
Reference
- Chiapasco M et al. Clinical outcomes of GBR procedures to correct peri-implant dehiscence and fenestrations: a systematic review. Clin Oral Implants Res 2009; 20: 113-123. https://doi.org/10.1111/j.1600-0501.2009.01781.x
- Clavero J et al. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: Comparison of donor site morbidity and complications. Clinical Implant Dent Relat Res 2003; 5: 154-160. https://doi.org/10.1111/j.1708-8208.2003.tb00197.x
- De Hua-Li: Management of bone defects in the aesthetic Congress scientific Report: EAO 24th Annual Scientific Meeting Stockholm 2015; 24-26.
- Garg AK: Grafting materials in repair and Quintessence 1999; 83-101.
- Geherke P, et al. Die drei-dimensionale Positionierung von Implantaten- Ein Fokus auf Aesthetik. Implantologie 2008; 16: 131-139.
- Happe A: Use of a piezoeletric surgical device to harvest bone grafts from the mandibular ramus: report of 40 cases. Int J Periodontics Restorative Dent 2007; 27: 241-249.
- Jensen OT: Alveolar segmental sandwich osteotomies for posterior edentulous mandibular sites for dental J Oral Maxillofac Surg 2006; 64: 471-475. https://doi.org/10.1016/j.joms.2005.11.030
- Trasarti S, Khoury Oral rehabilitation in patients with severe bone loss in the frontal area: clinical report on 10 consecutive treated patients. Clinical Oral Implant Res 2014; 25:Suppl 10, pag 24.
- Khoury F et al. Bone Augmentation in oral Quintessence Publishing 2007.
- Khoury et al. Mandibular bone block grafts: instrumentation, harvesting technique and J Parodontologi & d’Implantologie Orale 2006; 25:15-34.
- Khoury et al. Diagnostic and methods of intraoral bone Z Zahnarztl Implantol 199; 15: 167-176.
- Sohn Ds et al. Piezoelectric osteotomy for intraoral harvesting of bone Int J Periodontics Restorative Dentistry 2007; 27: 127-131
- Spin-Neto R et al. Remodelling of cortical and corticocancellous fresh-frozen allogeneic block A radiographic and histomorphometric comparison to autogenous bone grafts. Clinical Oral Implants Res 2015; 26: 747-752. https://doi.org/10.1111/clr.12343
- Spin_Neto R et al. Graft incorporation and implant ossointegration following the use of autogenous and fresh- frozen allogeneic block bone grafts for lateral ridge Clin Oral Implant Res 2014; 25: 226-233. https://doi.org/10.1111/clr.12107
- Tang YL et al. Ridge expansion alone or in combination with guided bone regeneration to facilitate implant placement in narrow alveolar ridges: a retrospective Clin Oral Implant Res 2015; 26: 204-211. https://doi.org/10.1111/clr.12317
- Zins JE et al. Membranous versus endochondral bone implications for craniofacial Plast Reconstr Surg 1983; 72: 778-785. https://doi.org/10.1097/00006534-198312000-00005
- Trasarti et al. Il prelievo di osso autologo da regioni intraorali con l’ausilio del Microsaw. Quintessenza Internazionale & JOMI n°4 2018.
- Sethi A. et al. Ridge augmentation using mandibular bone block grafts: Preliminary results of an ongoing prospective Int J Oral MAxillofac Implants 2001; 16: 378-388.
- Garcez-Filho J et al. Long-term outcomes from implants installed by using split-crest technique in posterior maxillae:10 years of follow-up. Clinical Oral Implants Res 2015; 26: 326-331. https://doi.org/10.1111/clr.12330








